by the
Consortium for the
Evidence-base practice of
Obstetrics
C.E.O. is dedicated to bringing science-based
maternity care to all childbearing women
A-C.E.O ~
The
American
College of
Evidence-based
Obstetrics
~
for
physicians who want to
re-establish
their profession as based on scientific principles
& reclaim their expertise in the use of physiological management for
normal birth
Stedman’s
Medical Dictionary definition of “physiological” – “…in accord
with or characteristic of the normal functioning of a living organism”
(1995)
Intro (similar to main
section of Position Paper) Chapters
one thru 6 (all new material)
most recent edited version ~
5/14/2004
21st
Century Maternity Care ~
Meeting the needs of our childbearing population
while remaining competitive in a global economy
Introduction
|
Preserving
the health of already healthy mothers and babies
is the primary role of maternity care.
Traditionally
this has been accomplished by
protecting mothers and babies from the rare mistakes of Mother Nature and
the frequent excesses of 20th century obstetrics. |
 |
The classic method for serving healthy childbearing women
is known as "physiological management". Its
classic principles are
“…in accord with, or
characteristic of, the normal functioning of a living organism”.
|
In this
science-based system,
physicians and midwives all over the world are taught to utilize physiological management
for normal pregnancy, labor
and birth. These
protective methods include a commitment not to disturb the natural process.
A
non-interventive approach
includes continuity of care, patience with nature, one-on-one social
and emotional support, non-drug methods of pain relief
and the right use of gravity. Obstetrical intervention is reserved for
complications or if the mother requests
medical assistance.
|
These physiological
principles provide the safest and most cost-effective
form of maternity care.
According to
the World Health Organization,
it is
the preferred standard for healthy women.
W.H.O. refers to
this as the "social" model of childbirth;
most countries depends on these
low-tech / high-touch methods to
provide cost-effective care. |
 |
In the US, this
is often called "Family-centered" or "Mother/baby/father-friendly"
maternity care. Approximately 70% of
pregnant women in the United States are healthy and have normal
pregnancies. That is approximately three millions normal births
annually. |
Mastery in normal childbirth services means
bringing about a good outcome without introducing any
unnecessary harm. Our
present system of obstetrics for normal childbirth does not do this very well.
In fact, our maternal-infant mortality record
has been
remarkably dismal throughout the 20th
century. This is
because obstetrical interventions,
originally developed for complications, are inappropriately used on healthy
women. This frequently introduced unnatural risks and
unnecessary complications. These
avoidable problems disturb the normal biology of labor and birth by routinely
applying of medical and surgical interventions to nearly 100% of the
childbearing population.
In spite of spending more money that any other country in the world,
the United States is 14th in maternal mortality and 22nd (third from bottom)
in perinatal mortality. The five countries with the best mother-baby outcomes
only spend a fraction of the money we do. These countries all have national
maternity care systems that depend on physiological management for healthy
populations.
To determine the quality of care received by mothers
in the US, the
Maternity Center Association of NYC recent surveyed healthy women with normal
term pregnancies who gave
birth in the previous 24 months.
The survey revealed than an average of seven or more serious medical or surgical procedures performed on each laboring woman
('Listening To Mothers'
survey by the
Maternity Center Association
of NYC, October 2003).
That means about three million healthy
childbearing women exposed annually to unnecessary obstetrical interventions. healthy childbearing women have been unwitting
subjects in an unregulated medical experiment without truly informed consent
for more than a century. This is a long history of non-consensual medical treatment.
A healthcare system that over treats three-quarters of its
patients is both expensive and dangerous. It exposes mothers and babies to
unnecessary physical and mental suffering and increased rates of preventable
death and disability. Recently the obstetrical profession
has upped the ante by promoting the strange idea that an 'elective', or medically unnecessary,
'maternal choice' cesarean is safer than normal childbirth. Many in the
obstetrical profession predict that cesarean delivery will completely replace
normal birth within the next 10 or 15 years to become the official "standard
of care".
However, medical journals make it clear to all that routine
obstetrical intervention for healthy women and birth conducted as a surgical procedure
is always more dangerous than the use of
physiological principles with appropriate social and psychological
support. Scientifically-speaking, this is not a controversial finding.
Reliable scientific evidence is neither lacking nor incomplete, nor is this
data the subject
of methodological disputes.
This irrational and unscientific system misdirects scarce
economic and human resources that could more properly be used to treat the
ill, the injured and the elderly. All forms of healthcare combined accounts
for 17% of the Gross National Product. Obstetrical care
accounts for 1/5th of the entire health care budget (equal to 3.4% of our
GNP). Seventy percent of those maternity care expenses are inflated by
unneeded medicalization which generates additional (and expensive!)
complications.
The bill for this failed medical experiment is being passed
on to the public and to
employers through the Medicaid tax burden and the increased cost of health insurance. In
order to remain competitive in the global economy, many industries are outsourcing manufactured goods and
replacing service jobs with off-shore workers. Economists have identified our inflated health care costs
as a major factor in these cost-cutting measures that depress our economy and
deprive American of much needed employment.
|
To meet the practical needs
of childbearing families while remaining competitive in the global free market,
the US must utilize this same efficacious form of maternity care as the
countries with the best, most cost-effective outcomes. An
improved and cost-effective system would permit limited health care
dollars to be properly used to meet the needs of the medical of the
truly ill. Compassionate, effective and
affordable maternity care is to the mutual benefit of mothers, babies,
fathers, families and society in general. |
 |
|
 |
The challenge for the 21st century is to bring
about a fundamental change in maternity care in the
United States. Normal childbirth services for healthy
women must be scientifically-based, compassionate and fiscally sound. This rehabilitated policy would integrate the classic principles
of physiological management with the best advances in obstetrical medicine
to create a single, evidence-based standard for all
healthy women used by all maternity care providers. |
|
Navigational Short Cut to
Chapters |
|
One ~ How
Did Things Go So Wrong?
Two ~
The
uncritical acceptance of an unscientific system of maternity care
Three ~ What
happens when the essential elements of success are missing
Four ~
Flat Earth Obstetrics -- a prisoner
of its own project
Five ~
Faith-based
Journalism ~a lose/lose proposition
Six ~ How to Make the System work for everyone
Physiologically- sound
practices (midwifery principles of care)
include: |
Chapter One
-- How Did Things Go So Wrong?
"the hallmark of obstetrical quality is the
prevention of the rare disaster
rather than the optimal conduct of the many normal cases"
[Dr. Brody 1981]
"Obstetrics has been rated as the
least scientifically-based specialty in medicine" [Dr
Ian Chalmers 1987].
Obstetrics is an important surgical
specialty originally developed in Europe during the 17th and 18th century. It
was a logical response to the pathological conditions associated with
pregnancy complications, obstructed childbirth and other reproductive
abnormalities. When mothers or babies need to be rescued from life-threatening
complications, modern obstetrical medicine does a technically superb and
compassionate job. None of us would choose to live in a world without its
pain-relieving and life-saving capacity.
In the last hundred years obstetrics for healthy women
has devolved into an ideology similar in its effect to a political or religious point of view.
This ideology gives rise to the illogical conclusion that
normal childbirth requires a constant stream of technological surveillance and
medical & surgical interventions. An irrational exuberance for all things
medical, combined with the rejection of other points of view, is detrimental to the goal of safe
and cost-effective maternity care. Obstetrics
is an “expert” system that has failed most in the very area it
was supposed to have the most mastery and expertise -- preserving
the health of already healthy mothers and babies. An operative rate well over 50% confirms that the introduction of harm has been
institutionalized and thus the obstetrical profession has failed in its most
basic responsibility --- “in the first place, do no harm.”
Obstetric ideology prefers a rigid moralistic vocabulary. It gives rise to a black/white,
right/wrong view of the topic that defines technology, drugs, medical interventions
and surgical procedures as right and safe, while implying that all other options
are wrong and dangerous. In the last fifty years, the onward march of obstetrical intervention
has progressed from the “knock’em out, drag’em out” style of the 1940s, 50s
and 60s to the "maternal choice" cesarean of our times. This progressive
medicalization started in the early 1900s with the routine use of ‘twilight sleep’ (i.e., narcotics and
amnesic drugs), general anesthesia, episiotomy, forceps and manual
removal of the placenta. Until the 1970s, the Cesarean rate remained under than
5% while instrumental delivery (forceps) and episiotomy was more than 90
percent.
|
In the last three decades, obstetrical medicalization
has changed in many ways but it is still an aggressive and interventionist model. In the year 2000 more than
50% of labors
were routinely induced or accelerated with Pitocin. Epidural has replaced
general anesthesia as the norm; the cesarean section rate for 2002 was 26.1
percent (26.8% in California). Too many normal pregnancies culminate with the
same operative delivery techniques used in the 1950s -- episiotomy and forceps
(or vacuum extraction) -- and healthy babies spend time in the neonatal
intensive care unit as a result of breathing problems or birth injury. This mismatch of care is expensive and
harmful.
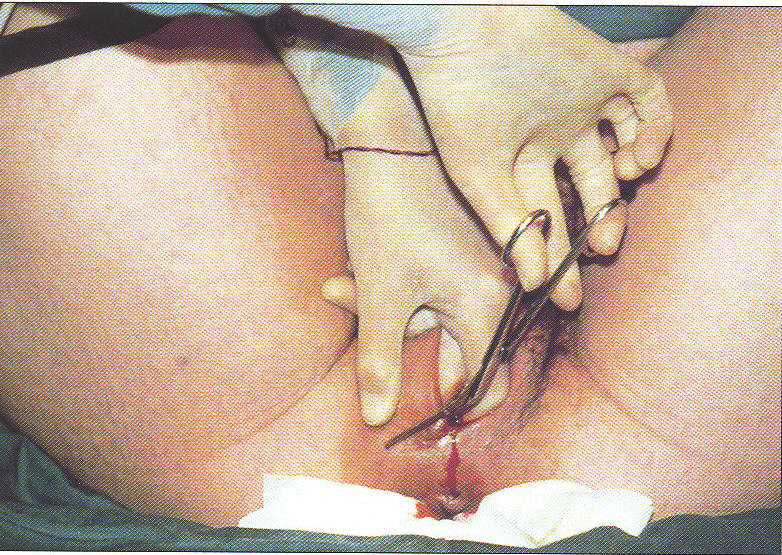
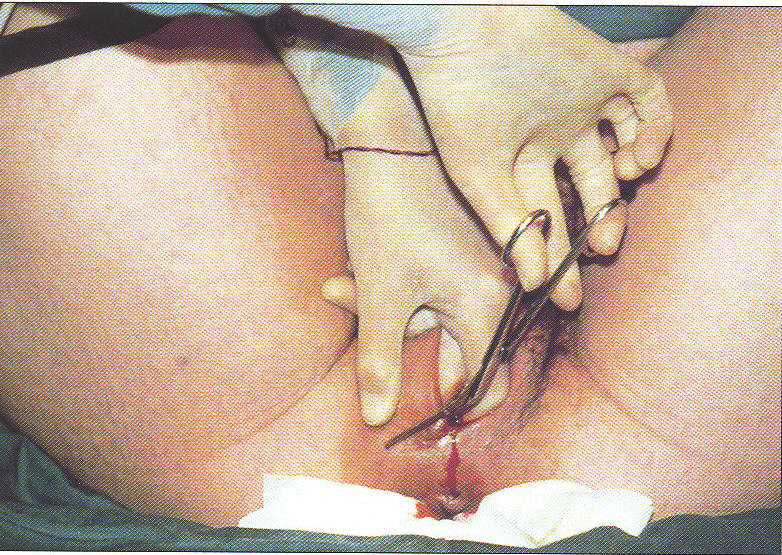
Photo of
Vacuum Extraction Delivery |
 |
The most recent expression of this
irrational exuberance for surgical intervention is a media
campaign by the obstetrical profession to promote the notion that an 'elective', or medically unnecessary,
'maternal choice' cesarean is safer than normal childbirth. This
public-relations campaign was topped off on October 31, 2003
by a press release
by the
American
College of Obstetricians and Gynecologists’ (ACOG). It reported a
decision by their Ethics Committee that is was "ethical" (based on ACOG's
professional code of ethics) for obstetricians to perform medically unnecessary cesarean
surgeries.
This strange
conclusion is the
predictable outcome of a century-long
PR campaign by organized
medicine. Beginning in
1910, the formal
strategy of the obstetrical profession was to discredit physiological management
as old-fashioned and dangerous
and replace
it with the idea that normal birth was now a surgical procedure
to be
performed by doctors. According to this dubious theory, childbearing was inherently
pathological. Physiological methods
were portrayed as inadequate and no longer to be tolerated by an enlightened medical profession and
a discerning public. This propaganda
exploited the lay public's lack of scientific
knowledge about normal birth, combined with an unquestioned faith in medical "science".
The belief that normal childbirth was inherently
dangerous gave rise to an unregulated medical experiment --
interventionist obstetrics as the norm for healthy women with normal
pregnancies. No matter how logical and well-meaning
this theory seemed originally, the unintended consequences of it were
negative and far-reaching. In the United States, organized
medicine built an
obstetrical care system in the early decades of the 20th century based on the
idea that every pregnancy was a “nine-month disease” that required a surgical
solution. The obstetrical profession has never
reassessed this untested hypothesis, which continues to underpin their
interventionist philosophy today.
However, approximately 70% of all pregnancies are
normal and occur to women who are healthy. Healthy women do not benefit from a medical
regime that disturbs the spontaneous biological process.
The principles of physiological
management -- i.e., care "in accord with, or characteristic of, the
normal functioning of a living organism"--
provide the safest and most cost-effective form of care for a healthy
population, regardless of the category of caregiver (doctor or midwife) , the
educational status of the practitioner (OB, FP, CNM or LM.) or the location chosen by the
parents (hospital, home or birth center).
Historical
knowledge-base destroyed
and traditional forms of care replaced
The obstetrical profession’s age-old denunciation of
midwives is a result of their peculiar
world view that defines normal childbirth as abnormal. Organized medicine’s Hundred Years' War on midwives
was the occupational equivalent of an ethnic cleansing. The stated objective
was to erase from the
scientific literature the institutional memory of the physiological principles
and the traditional skills used by midwives to facilitate normal childbirth. This resulted in an obstetrical
Dark Ages, aptly described as flat earth obstetrics, that has
spanned the entire 20th century.
Flat earth obstetrics
is the belief that unnecessary medical and surgical interventions are
necessary in every normal childbirth, despite evidence that such a policy is harmful. The
term is derived from the insistence by religious and political leaders
during the Dark Ages that the earth
was flat despite
evidence to the contrary.
|

Forceps Delivery |
Flat
earth obstetrics believes that every healthy woman inevitably benefits from
the care of a surgical specialist. This introduces harm by exposing
healthy mothers and their unborn babies to unnecessary,
potentially risky interventions while depriving them of the
protective and preventive strategies of physiological management.
Interventionist
obstetrics is failure by design, as such a design applied to a healthy population
can only fail.
It is a one-two punch that consists of absence of the right stuff
along with the unwarranted and unhelpful use of the wrong stuff.
|
The greatest realistic
danger today for healthy women who are well-fed, well-housed,
well-educated, and well-cared for during pregnancy is obstetrical
over-treatment and its many complications. For a healthy woman, her most
pressing needs during a normal pregnancy are primarily social and
psychological. Relative to labor and
birth, her greatest needs are met by the philosophy and principles of
physiological management which includes
continuity of care and the full time presence of a skilled and
supportive practitioner during active labor. Physiological management depends
on the
right use of gravity to naturally promote progress and continuous one-on-one labor support
to help
the mother cope without having to resort to the use of drugs. This strategy avoids the multiple side effects and complications that
accompany artificial hormones, narcotics, anesthesia and operative delivery.
The negative influence of flat earth obstetrics is amply
documented in historical sources, scientific studies, professional journal
articles and insider reports. Merely reading the headlines from
Ob.Gyn.News,
the largest trade paper for American obstetricians, shows how the insider
story, written by and for obstetricians, is far different from the
one promoted in the public press. While the obstetrical profession
thinks of its practice as logical, science-based and safe, the actual facts
reveal this form of routine interference in normal pregnancy and birth
to be illogical, unscientific and harmful. The
scientific method requires the burden of proof to falls on those who develop a new theory to establish its
merits before they can claim its superiority or usurp the original method. Scientifically-speaking, 20th
century obstetrical care by surgical specialists for healthy women is a failed medical experiment
as judged by the scientific method.
Reform is long over due.
Chapter
Two -- The
uncritical acceptance of
an unscientific system of maternity care
For the last century, scientific analysis of
interventionist obstetrics for healthy women has never been able to
demonstrate superior outcomes. Worse yet, scientific studies and vital
statistics between 1910 and 1930 show a 15%
annual increase in maternal deaths for more than a decade and
a 44% increase in neonatal birth injuries over the same period. The
escalating rate of mortality and morbidity was the direct result of
replacing the safer, physiologically-based care of midwives by obstetrical
interventions which included the routine
used general anesthesia, episiotomy, forceps and manual removal of the
placenta.
However, the poor statistical
showing of obstetrics has always been interpreted to mean that the
prevailing level of intervention was inadequate. Thus the statistically-documented
failure of interventionist care has actually spurred an ever-increasing
rate of medical and surgical interventions, up to and including the
“prophylactic
cesarean.” This is not a criticism of obstetrical care for women
with high-risk pregnancies and serious complications, for
whom interventionist care can be life-saving.
Tactics
properly reserved to treat obstetrical complications and emergencies have instead become an
all-purpose strategy for providing care to the entire population of
healthy patients. An example of confusion between tactics and strategy would be attempting to
use the tactics of war against an armed enemy as a strategy for
maintaining peace in a civilian population. Interventionist obstetrics for
healthy women with normal pregnancies adds unnatural dangers
to otherwise normal biology. It advances a false and misleading claim of value
added over that of physiologically-based care. In reality,
obstetrics for healthy women is an inefficient, value-subtracted system.
The promotion of interventionist obstetrical care for healthy women by ACOG is
a false and misleading claim.
Without truly informed consent, healthy childbearing women have been unwitting
subjects in this medical experiment for more than a hundred years. This
equates to non-consensual medical treatment. The bill
for this failed medical experiment is being paid by the public and by
employers through the increased cost of health insurance and the Medicaid tax
burden. Our inflated health care costs are identified by economists
as a major reason for employers to choose cost-cutting measures, such as outsource manufactured goods and
replace service jobs with off-shore workers, so as to remain competitive in
the global economy.
|
Contemporary obstetrical practices for healthy women were
founded on a 19th century reductionist view of childbirth.
In a reductionist view, the rich tapestry of childbearing, with its
emotional nuances and long-term social consequences, is reduced to
mortality statistics. |

Internal electronic fetal monitor
attached to unborn baby's head by screwing an electronic spiral
wire into the baby's scalp |
Since childbirth is a fundamentally successful biological system, healthy
mothers and babies generally survive and leave the hospital alive -- the medical
definition of a 'success'. But in the reductionist view, physical or psychological damage to mother or baby
(such as operative or instrumental delivery) and unmet social and
psychological needs are not factored into the equation. |
In addition, the profession of obstetrics is
inextricably mixed up with childbirth services as the huge and lucrative
'baby business'. A revealing example of this can be seen in the following
excerpts from Ob.Gyn.News on the off-label use of misoprostol to induce
labor. Misoprostol (trade name 'Cytotec') is a drug marketed to treat stomach
ulcers. When used in obstetrics, it is associated with an increased rate of
uterine rupture. None the less, Dr. Maslow, director of maternal and fetal medicine at the
Geisinger Health System in Danville, Pa. is rhapsodic in his
description of the financial advantage to the hospital industry when normal
birth is managed as a form of 'Agra-business'. Just as hormones are used to
boast egg & dairy production and to speed up the weight gain of cattle, so too the obstetrical
system uses artificial hormones to manipulate birth-related body
functions. This permits them to put biological processes on the clock, so they
are
more convenient and profitable for the institution:
"Oral misoprostol is far and away the most cost effective
labor induction methods, Dr Arthur S. Maslow asserted at meeting ....
The best part about it is that you can block-schedule your nurses so
that you have enough on hand. With a 90% successful induction rate within 8-10
hour, if we start our inductions at 7 a.m., we know that we're going to have X
number of patients being admitted by 4 p.m. That's helped our hospital
tremendously," said
Referring to the drug misoprostol, Dr Maslow remarked:
"Its a great agent. It works very, very efficiently. Its
very safe ..... And its ungodly inexpensive: 27 cents per tablet. At
the most we use two or three tablets. "
Discussing of how Cytotec / misoprostol induction is best
managed, Dr Maslow had this advise: ...
" ....the patients arrive at the antepartum diagnostic
center first thing in the morning .... given a single oral 50-ug
tablet..... monitored for the next hour .... Then we make them walk for 2
hours. They can stay in the hospital, go to the mall, I don't care.
Just don't rest them during an induction. You're killing your hospital
financially if you do that, just killing them. Its not fair to the hospital
......."
The cognitive distance between the woman's view of
her maternity care and the medical-industrial complex's view is huge. The
obstetrical profession sees childbirth from the same narrow
perspective that infertility specialists see conception. Since making love and
being artificially inseminated both result in pregnancy, they make no
distinction between the two. This depressing
situation is the predictable consequence of purposefully preventing the
corrective and humanizing influence of physiological management from being applied to the field of
normal maternity care.
Midwifery management, which
depends on physiological principles, and interventionist obstetrical
care both produce equal results as measured by
babies born alive and without neurological damage. What is remarkably different and
missing from obstetrical management is the opportunity to address the full
spectrum of maternal, infant and societal needs. Pregnancy "produces a mother as well as a baby".
Good
maternity care should address the all these needs-- physical,
psychological, social and developmental, especially as it relates to preparing
women to mother
their new baby. In the physiological model, the interests of
the mother are not seen as in conflict with those of the baby. Instead the
mother-baby are seen as a unit or couple with complimentary needs. With rare
exception, what is good for mothers is directly or indirectly good for their
babies.
What
works and why bother ...
|
At present, it is virtually impossible
for healthy families to get the safe care they deserve from hospital-based
obstetrics. As contrasted with
the medical model, physiological
management of normal labor is protective of both mothers and babies, reducing
the surgical rate from over 50% to under 5%, with
equally good perinatal outcomes. These
protective methods, as provided by midwives and a small number of
physicians, include
a commitment not to disturb the natural process.
Its principles
constitute the "social" model of childbearing identified by the World
health Organization as the preeminent system to provide normal maternity
care. In the United States the social model is also known
as "family-centered" or "mother-baby-father friendly" maternity care. In
this system, professional caregivers
recognize that the integrity of the mother-child relationship begins in
pregnancy. The mother is not viewed as a "patient" in the sense of being
infirm or incompetent but rather as a competent and self-directed
individual. She is acknowledged as the "primarily" caregiver of her
baby, since it is the mother who voluntarily decides whether or not
to seek maternity care during pregnancy. It is normally the mother
who first notices an obstetrical problem, who voluntarily seeks out
medical assistance and ultimately, must give consent for invasive
medical and surgical treatment. It is appropriate for her good will
towards her baby to be assumed unless there is clear and obvious
evidence to the contrary.
|
 |
The principles of social or
'mother-friendly' model depend on:
-
a respect for and trust in
the normal biology of pregnancy and childbirth
-
an expectation of normalcy
in the progress of labor and birth
-
recognition of the mother's right to choose and
control the environment for labor
-
acknowledging the mothers' right to direct her
own activities, positions & postures during labor
|
Its practices include:
-
continuity of care
-
patience with nature
-
full-time presence of the
caregiver during active labor
-
continuous one-on-one social
and emotional support
-
appropriate physical and
psychological privacy for the laboring woman
-
non-drug
methods of pain relief such as walking, hot showers and deep water tubs
-
no arbitrary time limits as long as reasonable
progress, mom & babe OK
-
vertical postures, pelvic mobility and the right
use of gravity
-
maternal choice of birth position unless medical factors require otherwise
-
physiological clamping of
umbilical cord -- after circulation has stopped (+/-3 minutes)
-
immediate possession and control of healthy
newborn by mother and father
|
 |
The relationship of the social
model and contemporary medicine includes:
-
palliative treatment of
minor medical deviations
-
the capacity for
emergency-response by the practitioner
-
access to and appropriate
use of the obstetrical care system, drugs and
anesthesia when indicated
The elements of success for normal labor and
spontaneous birth are the same regardless of location -- home, hospital or
birth center. While physiological management of labor dramatically reduces the need for
pain medication or epidural anesthesia, the employment of
physiologically-sound methods does not prohibit hospitalized
mothers from receiving drugs and anesthesia as desired or required.
A socially appropriate
environment is one in which the mother feels unobserved and yet secure, with
emotional support as necessary. This is the purposeful mechanism of
physiological management that addresses the mother’s
pain, her fears and privacy needs so that labor can unfold naturally,
without the need for medical interventions and pain medications. It is also necessary to take into account the
positive influence of gravity on the stimulation of
labor, dilatation of the cervix and decent of the baby through the bony
pelvis. Maternal
mobility not only helps this process along but also diminishes the mother’s
perception of pain, perhaps by stimulating endorphins. To ignore the well-known
relationship of gravity to spontaneous progress is to do so at the peril of mother and
baby. The complex interplay of the physical and the psychological are such a
biological
verity of childbearing, that women have an undeniable right to have the maternity care
provided to them be structured to address both the gravitational and
psychological influence on the spontaneous biology of labor and birth.



Non-medical strategies that properly address these
gravitational influences and the psychology of normal labor are particularly effective in averting
episiotomy and operative deliveries and their subsequent complications, such
as pelvic
organ prolapse and incontinence. Normal management dramatically
reduces the cesarean rate, which also averts
the short and long-term sequelae of cesarean
surgery for both mothers and babies. Because cesarean surgery so greatly
increases maternal morbidity and mortality; the use of physiologic principles
reduces maternal morbidity and mortality for a significant number of
women.
Direct complications
of cesarean surgery for mother and baby include:
-
double or triple the risk of
maternal death
-
nine-fold increase in
potentially fatal blood clots
-
triple the risk for maternal
infection
-
maternal hemorrhage
-
13-fold increase in
emergency hysterectomy
-
higher risk of lung disorders and
operative lacerations for babies
-
Cesarean babies also suffer
increased rates of asthma as children and triple the rate of asthma as adults
Post Cesarean
complications associated with post-cesarean pregnancy, include:
-
secondary infertility
-
tubal (ectopic) pregnancy
-
increased miscarriage &
stillbirth
-
abnormal placentation (previa and
accreta / percreta
-
blood transfusions
-
uterine rupture
-
emergency hysterectomy
-
maternal and neonatal death
-
disability or neurological
damage to mother and/or baby
Healthy families seek out home-based midwifery services not because they are indifferent to the safety of their babies.
For many families, it is their only access to the safety of physiologically-based
maternity care. The best, perhaps the only, solution to the home
birth controversy is to make maternity care in homes and hospitals equally
safe and equally satisfactory so that families are not forced to choose
home birth for want of appropriate, compassionate and cost effective care in
hospitals. This leads us to the natural and compelling conclusion that our
current hospital-based maternity care system must be rehabilitated.
Chapter Three ~
What happens when the
essential elements of success are missing
In October 2002, a national survey
-- Listening To Mothers -- was commissioned by the
Maternity Center Association
of NYC. This was done in an effort to track contemporary obstetrical trends and the
quality of care received by healthy childbearing women. The MCA is a
non-profit organization that has been promoting safe maternity care since
1918. They also develop educational materials for expectant parents on ‘evidenced-based’
practices -- that is, maternity care policies that are based on a scientific
assessment of the safety and effectiveness of commonly used methods and
procedures.
The determination of scientific validity is based on the published work of
Drs Ian Chalmers and Murray Enkins. Their compendium, entitled “A Guide to Effective Care in
Pregnancy and Childbirth” (GEC), is the bible for evidenced-based
maternity care. A Guide
to Effective Care maintains a
review of all pregnancy and childbirth related studies published in
the English language in the last 30 years. It identifies six levels of
effectiveness & efficacy, ranging from the positive end of “clearly
beneficial” (category 1) to the negative end (category 6) of “likely to be
ineffective or harmful.” Using the preponderance of available evidence, Drs
Chalmers and Enkins rate the safety and efficacy of each standard maternity
care practice and each regularly used medical/ surgical intervention. Based on
these categories, the Guide to Effective Care cautions that:
"Practices
that limit a woman's autonomy, freedom of choice and access to her baby should
only be used if there is clear evidence that they do more good than
harm"
"Practices
that interfere with the natural process of pregnancy and childbirth should
only be used if there is clear evidence that they
do more good than
harm"
The
Maternity Center Association documented a "significant gap between
scientific evidence and standard obstetrical practice." According to
teaching materials by the MCA: "Healthy, low-risk
women in the United States often receive maternity care that is not consistent
with the best research". Using the rating system recommended in the Guide
to Effective Care in Pregnancy and Childbirth , laboring women in the US are routinely exposed to a plethora
of practices officially categorized as
of “unknown or unproven
effectiveness,” “unlikely to be effective,” or
“known to be
harmful.”
According
to the MCA, many people are not aware of the following major areas of concern:
-
The under-use of certain practices that are safe and effective
-
The widespread use of certain practices that are ineffective or
harmful
-
The widespread use of certain practices that have both benefits and risks without
enough awareness and consideration of the risks
-
The widespread use of certain practices that have not been adequately
evaluated for
safety and effectiveness
The Listening to Mothers survey revealed that 99% of healthy pregnant women do not
receive science-based maternity care from their obstetrical providers. An
average of seven medical or surgical procedures was performed on each healthy
woman giving birth in the 24 months preceding the survey. They reported
that there were virtually no spontaneous, unmedicated births (i.e., without
medical or surgical interference) in institutional settings. Only 1% of
this cohort of healthy women were not subjected to institutionalized interference and
those were the 1% who gave birth at freestanding birth centers or at home.
Intervention
statistics from the MCA's survey of healthy women who delivered at term in the last 24 months:
93
%
exposed to continuous electronic fetal monitoring (associated with
increased CS rates)
86 % had IVs while being prohibited from drinking or eating
74 % required to give birth lying on their back (increased
fetal distress, instrumental and operative delivery)
71 % immobilized / confined to bed / not permitted to walk during
labor (dysfunctional labor,
increased pain)
67 % had artificial rupture of membranes (increased
prolapsed cord, infection)
63 % had labors induced or accelerated with prostagladins and/or artificial
oxytocin (Pitocin),
63 % had epidural anesthesia (increased
instrumental delivery, CS)
58 % had a gloved hand inserted into their uterus after birth (increases
bleeding & uterine infection)
52 % had bladder catheterizations (increases bladder / kidney
infections)
35 % had episiotomies (increased
bleeding, pain, infection, sexual dysfunction)
24 % had cesarean surgery (increases maternal mortality 2-4 times)
13 % delivery by forceps or vacuum extraction (increased
fetal & maternal damage, long-term incontinence)
The total
operative delivery was 37%
excluding
episiotomies,
72% if episiotomies are included. It should be noted that these statistics are
for healthy women at term with normal pregnancies. Intervention rates are much
higher for women with premature labor, multiple pregnancies or medical
complications. This accounting is consistent with data from the
CDC’s National Center for Health Statistics Vol. 47, No 27, The Use of
Obstetric Interventions 1989-97, which documents a steady annual increase
since 1989 in each of these major interventions.
In
light of these results, the
Maternity Center Association recommended “more physiological and
less procedure-intensive care during
labor and normal birth”.
However, it must be noted that interventionist obstetrics makes its
money from 'billable units' -- i.e., medical and surgical procedures
performed.
Other
Voices, Other Issues, Same Miserable Story
In an article entitled "Elective
Cesarean Section: An Acceptable Alternative to Vaginal Delivery?", Dr
Peter Bernstein, MD, MPH, Associate Professor of Clinical Obstetrics &
Gynecology and Women's Health at the Albert Einstein College of Medicine, also
reported on the failure of the obstetrical profession to practice evidence-based
medicine.
Addressing the popular notion that pelvic floor damage and incontinence were the
inevitable result of normal birth (to which cesarean surgery was the proposed 'solution'), Dr Bernstein observed:
"these adverse side
effects may be more the result of how current obstetrics
manages the second stage of labor. Use of episiotomy and forceps has
been demonstrated to be associated with incontinence in numerous
studies. Perhaps also vaginal
delivery in the dorsal lithotomy position [lying flat on the back] with encouragement from birth
attendants to shorten the second stage with the Valsalva maneuver
[prolonged breath-holding], as is
commonly practiced in developed countries, contributes significantly to the
problem."
To
address the discredited idea that cesareans protect the mother from surgery later in
life to treat organ prolapse
or incontinence, another obstetrician
wrote that: " [physicians] would
have to do 23 C-sections to prevent one such surgery
." [Dr. Elaine
Waetjen, Ob.Gyn.News; August 1, 2002, Vol 36, No
15]
The May 2004 edition of ObGynNews noted that elective
cesarean is riskier to the newborn baby than vaginal birth. It stated:
"Neonates born by elective cesarean section are at greater
risk of poor outcomes than those born vaginally.... 14% of those
from the elective cesarean group (relative risk 3.58) were admitted to an
advanced care nursery [in contrast with only
5% of vaginal delivery] ....oxygen was used ...
in 73% of those in the elective cesarean group
[compared to only 23% in vaginal delivery group]...
The difference may be
due to beneficial effects of the process of labor and delivery on infants
and their ability to transition following delivery. Clinicians should
consider neonatal effects, as well as maternal well-being, when discussing
the possibility of elective cesarean delivery inpatients with uncomplicated
pregnancies, he said."
[emphasis added]
(ObGynNews May 1, 2004, Vol 39, No 9)
In regard to the topic of medically
unnecessary elective or 'maternal choice' cesareans, performed in a misguided
attempt to reduce pelvic floor dysfunction, Dr.
Peter Bernstein noted:
There may be
no legal
liability to the physician who performed the patient's first cesarean section
when the patient winds up with a hysterectomy or worse, but that does not clear
that physician of responsibility for performing a surgical procedure of
unclear benefit upon a patient's request.
Some argue that, from an
ethical point of view, allowing a patient to choose to deliver by cesarean is
not substantially different from allowing her to choose to undergo cosmetic
surgery. But cesarean is very different. The benefits of elective cesarean
relative to vaginal delivery are not established and the risks are
substantial, especially given the potential for future repeat cesareans.
That women are seeking
elective cesarean deliveries is probably more significant in that it indicates
the failure of modern medicine and society at large in the sense that
women may fear the experience of labor
and birth attendants may fear the legal
risks of allowing appropriate women to have a trial of labor.
Episiotomy -- the "unkindest cut"
The evidence against routine use of episiotomy is irrefutable --
it fails to help and it directly produces harm. It is referred by some in the
medical literature as an "injurious procedure".
According one physician-researcher, Dr. Robert
Woolley, MD" "...
there are are
no valid indications, maternal or fetal, for
episiotomy, and therefore the only appropriate rate of its use is
zero."
In regard to a startling
lack of informed consent, Dr. Woolley quotes and affirms author Shelia
Kitzinger, stating that: "
... episiotomy 'is the only surgery likely to be performed without her
consent on the body of a healthy woman in Western society' (Kitzinger 1986
Intro). It is puzzling and troubling that this is so."
Excerpts from "Benefits and risks of episiotomy:
A review of the English-language literature since 1980"
by Robert
Woolley;
If we were to adopt a more scientific view of the evidence
available on the subject of episiotomy, disclose this information to our
patients, listen to their perspective, and ... choose to heed the
evidence over our prejudices, we could hardly fail to reduce
dramatically the use of this injurious
procedure.
It is axiomatic in our profession that the burden of proof of the
safety and efficacy of a surgical procedure falls on those who perform
or advocate it. This burden clearly has not been met for episiotomy
;
its safety and efficacy had not been demonstrated ..... why
has practice not changed?
If episiotomy were a new, experimental
procedure, and its initial results those described in this review, there
can be no doubt that the research would be halted and episiotomy
relegated to a brief and ignominious place in the annals of medical
history.
The English-language literature published since 1980 on the benefits
and risks of episiotomy can be summarized as follows:
Episiotomies prevent
anterior perineal lacerations (which carry minimal morbidity), but fail
to accomplish
any of the other maternal or fetal benefits traditionally
ascribed, including prevention of perineal damage and its sequelae, prevention
of pelvic floor relaxation and its sequelae, and protection of the newborn
from either intracranial hemorrhage or intrapartum asphyxia.
|
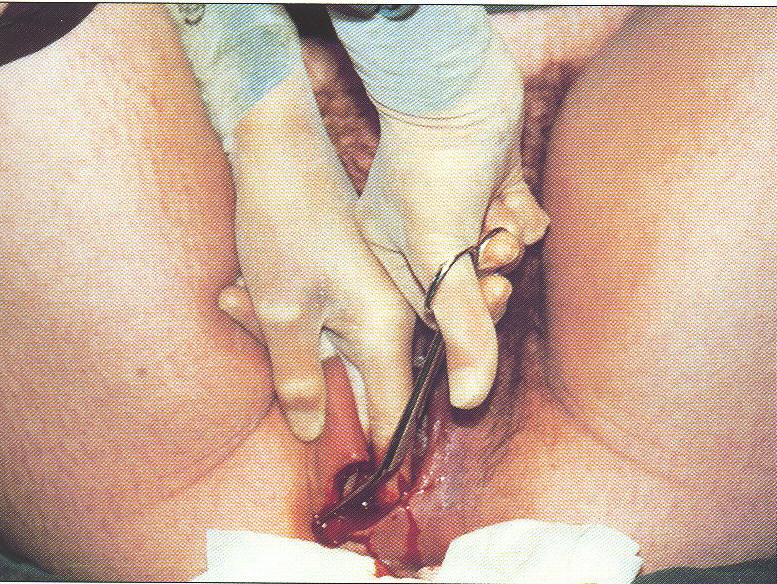
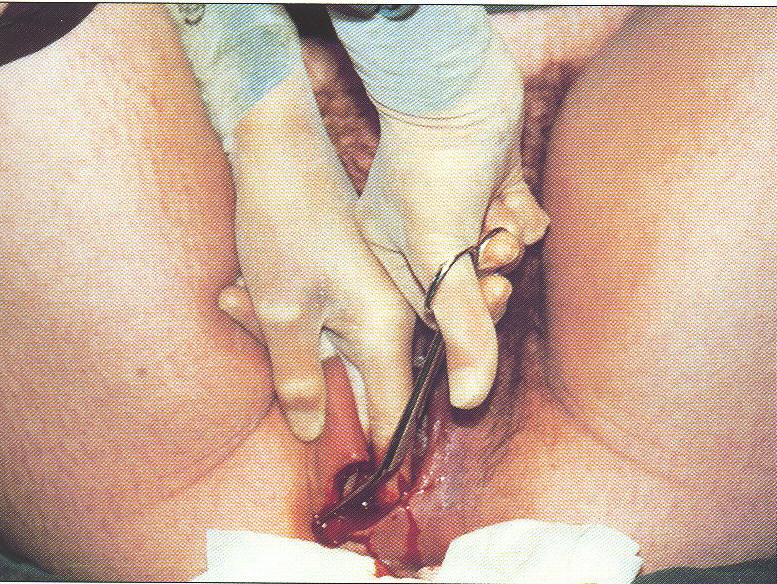
Textbook
pictures instructing medical students in the surgical technique of
Episiotomy -- an incision
into the vagina during the pushing phase of childbirth. It is never
medically necessary unless the
unborn baby is distressed or if the
mother is exhausted and asks for an
episiotomy to shorted pushing. |
|
 |
 |
|
blades of the surgical
scissors
inserted into vagina |
surgical scissors
closed so as to
create a 2-3 inch incision |
In the process
of affording this one small advantage, the incision substantially
increases
maternal blood loss, the average depth of posterior perineal injury, the
risk of anal sphincter damage and its attendant long-term morbidity
(at
least for midline episiotomy), the risk of improper perineal wound healing,
and the amount of pain in the first several postpartum days.
The most famous shibboleth of medicine, "Primum non nocere" ("First,
do no harm") — that is, the assertion that the avoidance of inflicting
any harm outweighs all other moral imperatives — probably has neither the
historical nor the philosophical weight we tend to attribute to it [187-188].
Nevertheless, the principle of non-maleficence remains foundational to
our professional ethics.
We would do well to "provide patient care in the
spirit of a new aphorism, based on the concept of risk-benefit analysis: Saltem plus boni quam mali efficere conare — At least try to do more good
than harm" [189]. By either standard,
episiotomy has "been weighed in the balance and found wanting".
Excerpts from "Benefits and risks of episiotomy: A review of the English-language literature
since 1980".Dr.
Robert
Woolley, MD
Part I. Obstet Gynecol Survey 1995; 50:806-820; Benefits and risks of episiotomy: A review of the English-language literature
since 1980. Part II. Obstet Gynecol Survey 1995; 50:821-835 and
unpublished manuscript circulated on Ob.Gyn.Net user group (1997)
Neonatal Consequences of Epidural Anesthesia
The newborn complications
of epidural anesthesia
are rarely discussed in public. However a study
entitled "Epidural, maternal fever and neonatal sepsis evaluation"
by Dr Ellice Liaberman, et. al.
[published
Pediatrics, 1997;99:415-420]
reveals the astonishing proportion of
iatrogenic complications affecting babies that are directly related to the
use of these anesthetic:
Overall, 63% of the women (1,047) studied received epidurals, but their
number accounted for 96% of those who developed fevers during labor.
Their babies accounted for around 86% of all newborns tested for sepsis
and about 87% of those given some
form of antibiotics.
This means 87% of neonatal admissions to special care nurseries for
antibiotics are a direct complication of epidural use -- a huge and
unnecessary financial expense added to the bill for "normal birth" services.
In addition, it appears that the body temperature of the unborn baby can be
raised to dangerously high level when its mother has an epidural:
One study measuring fetal skin
temperature during labor found that in 9% of the cases reviewed
where the mother was given an epidural, fetal skin temperature reached
39 degrees centigrade [approximately 103.6
degrees F], as compared with the non-epidural group in
which no fetuses had as high a skin temperature.
They suggest that as fetal core
temperature is likely to be 0.75 degrees C. [approx. 1 1/2 degrees F.]
higher than fetal skin temperature, core temperature
[of the baby] may sometimes reach 40
degrees C. [approx. 105 degrees F.], a
temperature that in adults is associated with heat
stroke risk.
The lead author of this study, Dr. Liaberman
addresses the topic of these complication for the new baby and the need for
fully informed maternal consent based on knowledge these possible
complications. She says that she:
".... does not want to stress-out young mothers-to-be with her findings, but
feels all women should have this information when deciding on an epidural."
"The testing process to see if the newborns have sepsis
[infections] is extremely painful
because it involves drawing vials of blood and sometimes doing a lumbar
puncture [spinal tap] to remove fluids from the infant's spine," she said.
"It can become an ordeal for the infant."
Chapter Four ~ Flat
Earth Obstetrics
-- a prisoner of its own project
And yet, when the obstetrical profession is presented with this corrective information, it
consistently fails to
take corrective action. It is a
prisoner of its own project – the
ever-expanding medicalization of normal birth based on the discredited notion
that childbirth is a fundamentally pathological event requiring medical
management and surgical delivery. In spite of the mass
of scientific literature documenting these iatrogenic complications, the obstetrical
profession refuses to be held accountable, or even to acknowledge, the
problems it
systematically introduces into the care of healthy childbearing women. Instead it
claims that the biology of normal childbirth itself is intrinsically defective
and that complications, such as pelvic floor damage and incontinence, are
merely the 'collateral damage' of normal vaginal birth and
certainly not to be associated with their interventionist management style. According to
ACOG, the "smart" choice -- often referred to by obstetricians as “vaginal
by-pass” surgery -- is to avoid these problems via the elective and medically
unnecessary cesarean.
The problem is that physicians
are the natural spokespersons for the scientific discipline of medicine. This
places a societal burden of candor and accuracy on doctors by virtue of their advanced education
and license to practice medicine and creates a higher standard of conduct than
mere recitation of personal preference or professional self-promotion. The
very fact that physicians are holders of a doctorate (a PhD) in the
science of medicine gives the public every good reason to believe
that formal statements made by physicians about matters of health, safety and
medical care are unbiased, scientifically-based and factually correct.
This would include a duty to communicate only scientifically valid information
in a public forum unless such statements are identified as merely a personal
or political opinion.
As amply demonstrated by the literature, many of those with a doctorate are not living up to their
obligation to speak and act on the best scientific evidence. It can
be argued that licensed physicians have a legal or "due diligence" obligation
to provide "honest, complete, and impartial" information in their
field of expertise.
ACOG policies define the ethical
responsibilities of an obstetrician giving "expert witnesses" in
court as a duty to provide "honest, complete, and impartial" testimony. The
American Medical Association considers the provision of "expert testimony" to
be a bona fide practice of medicine; physicians giving
fraudulent testimony can face disciplinary charges by their
licensing boards. So far, none of these noble ideals are being applied
to ACOG's public propaganda campaign, which focuses on promoting routine
medicalization, elective inductions and maternal choice cesarean delivery.
They pursues this self-serving agenda while actively deriding physiological
management as a either substandard or dangerous form of care.
Betrayal of Trust ~ the
all to familiar story of
big business being unaccountable to the public
While the motives are different, the methods used by
organized medicine are disturbingly similar to those used by tobacco
companies, Enron, Arthur Andersen and others who abuse the public trust.
The strategy depends on asymmetrical access and control of information
combined with the popular notion that expert systems are far too complex
for any layperson to understand. Asymmetrical information means that only
insiders have the full story. As insiders, they routinely conspire to conceal data and sources
that do not protect or promote their own interests. In the corporate and
political realm, it seems that only Martha Steward is expected to tell the
whole truth all the time. Everyone else depends on the
asymmetrical control of information.
Asymmetrical distribution
of vital information by the obstetrical profession raises this disturbing question:
"Do two, carefully chosen half-truths
equal Truth with a capital T or .....
is this a legal way to conceal
the greater Truth while not having to tell an outright lie?"
Unfortunately people assume that expert members of an expert system can
always be counted on to be above reproach. The public places such
trust in them that to most people, exerting oversight of expert
systems seems both unnecessary and frankly impossible.
And yet obstetrics
is an “expert” system that has failed most in the very area it
was supposed to have the most mastery and expertise -- preserving
the health of already healthy mothers and babies. As "experts" it was their
duty to protecting women from
the vagaries of Mother Nature and to guard women against the unwise meddling
and excesses of Modern
Medicine. Mastery in childbirth services meant
bringing about a good outcome without introducing any
unnecessary harm. An operative rate over 50% confirms that the introduction of harm has been
institutionalized and thus the obstetrical profession has failed in its most
basic responsibility --- “in the first place, do no harm.”
Midwifery -- Collateral Fatality to Flat Earth Obstetrics
For the entire course of the 20th century, the
obstetrical profession has distracted public attention from its unproven
hypotheses of ever-escalating intervention by redirecting everyone’s attention to the
supposed midwife problem.
The midwife problem was an invention of organized medicine which referred to
the problem that doctors were having in getting rid of midwives.
The straightforward purpose
of eliminating the practice of midwives was to commandeer normal midwife
births into “clinical material” (teaching cases) for medical students.
This was to
rectify glaring deficiencies in medical education as identified by the
Flexner Report, published in 1910, which investigated why maternal and
infant mortality in the U.S. was "appallingly high" compared to
other developed countries. Unlike the prestigious medical schools of
Europe, obstetrical education in the U.S. did not include clinical or hands-on experience at that time. The untested hypothesis by medicine school
administrators was that if
female midwives could do a decent job of delivering babies then doctors trained in surgery would be able
to do a vastly superior job if only they could be supplied with improved medical
education. The improvement they sought was a steady supply of teaching cases
(referred to as obstetrical 'material') that was needed
by medical students to “practice”
operative procedures (such as use of forceps) and to hone their clinical judgment. To
accomplish this ambitious goal, physicians embarked on an aggressive campaign to eliminate the
profession of midwifery.
The not-so-subtle hidden agenda was to
elevate
the social status
of obstetrics and the income of physicians. This was to be done by divorcing childbirth services
from the low paid work of women/midwives so that a 'professional' (i.e., much higher)
fee could be collected. The excuse used
in public for these radical changes was that it was unfair to the poorer class of women, who
commonly used midwives, to be deprived of anesthesia and other “benefits” of medicalized
childbirth. According to the obstetrical profession, the real reason
obstetric statistics reflected such poor
outcomes was because doctors were forced to take care of all the mistakes made by
midwives. They argued for a single standard of care -- a medically-based standard
defined by and for
doctors -- in which spontaneous childbirth was redefined
as a surgical procedure that could only be performed by a
surgically-trained specialist on an anesthetized mother in a properly equipped
operating room.
For women the midwife problem was not simply that doctors,
instead of midwives, were being employed to deliver babies. From the
perspective of history, the real midwife problem was that, in order to make midwives wrong, medical
politicians also had to make the entire discipline of midwifery itself wrong by deconstructing
the very foundation of normal birth-- the philosophy and
principles of physiological management.
Whatever midwives did, doctors had to do just the opposite. If the discipline of
midwifery related to childbirth in healthy women as a unique but nonetheless
normal biological
function, then obstetrics must relate to childbirth as uniformly abnormal and,
when speaking of
childbirth, always speak of the “danger of childbirth.”
In order to take patients--clinical material--from
the thriving midwifery practices of the early 1900s, medical politicians
publicly promoted the idea that obstetrician care was highly superior
to that of mere midwives, claiming that the lives of mother and baby were
vastly safer in the hands of doctors. As an
added inducement to the public to trade up to doctor care, it was
promised that the mother would be knocked out during birth with general anesthesia and not remember
anything – the original version of painless childbirth.
What started
out as a midwife problem quickly became a life-threatening medical problem for childbearing women and babies.
Instead of treating
childbirth as a normal body process, physicians related to the care of healthy
childbearing women as an opportunity to develop their skills in interventive
obstetrics by routinely using chloroform, episiotomy, forceps and manual
removal of the placenta at every normal birth. It
is no wonder that anesthetic deaths, hemorrhage, infection, neurological
injury to newborns and long-term gynecology complications for mothers followed
in the wake of these ill-conceived ideas.
When mothers or babies died or were
permanently damaged as a direct result of this unwise interference, the midwife problem became a
crisis for the rest
of society. In 1932 a physician-statistician for the
Metropolitan Life Insurance Company studied the care provided and the outcome
statistics for births attended by midwives from the Frontier Nursing
& Midwifery Service in the Appalachian Mountains of Kentucky. In a public address he
stated that if such midwifery care were generally available to the
childbearing women of the United States, it would
reduce the maternal/perinatal mortality by an estimated 70,000 deaths per year --
10,000 mothers, 30,000 stillbirths and 30,000 babies that died before they
were a month old.
["Into This Universe" , Alan Frank
Guttmacher, MD, John Hopkins University Viking Press, 1937, Charter 4, p. 329]
Despite such a stunning indictment, the obstetrical juggernaut continued.
Eliminating midwives also eliminated any useful comparison of the two different methods via analysis of
vital statistics derived from birth registration records. Without
data on midwife-attended births, outcomes of childbirth for healthy mothers with normal
pregnancies managed by physiological principles could not be contrasted with
outcomes following the use of interventionist obstetrical techniques on healthy
women. By controlling the public discourse through the control and asymmetrical distribution of
information, organized medicine ultimately came to control public opinion.
Thus the
profession of obstetrics also controlled the legal and legislative framework for how maternity care was
configured and provided throughout the 20th century.
One obstetrical spokesperson of the period (1911) summed up the
all-encompassing aspirations of the obstetrical profession this
way:
“We
believe it to be the duty and privilege of the obstetricians of our country to
safeguard the mother and child in the dangers of childbirth. The
obstetricians are the final authority to set the standard and lead the way to
safety.
They alone can
properly educate the medical profession, the legislators and the public."
Boston Medical and Surgical Journal, Feb. 23, 1911, page 261
However, the price for unconscious childbirth under
medical (interventionist) instead of midwifery (physiological) management
was staggering – an increase in maternal mortality (15% per year, usually
from sepsis or hemorrhage) and increase in neonatal birth injuries by 44% in the
first decade (1910 –1920). In addition to maternal death and infant brain
damage, women also suffered from pelvic floor damage such as fistulas and
incontinence subsequent to the damage from episiotomy and forceps, which
were routinely used on every mother who did not deliver precipitously before
the doctor arrived.
Chapter Five ~ Faith-based
Journalism ~a lose/lose proposition
Unsafe maternity care practices have dominated obstetrics
for the entire 20th century and yet have gone unnoticed,
unexamined and unchallenged in the public arena. Journalists have increasingly
accepted expert systems as beyond scrutiny and above reproach. This has produced faith-based reporting, in which journalists never look beneath
the surface. Based solely on obstetrical sources, print and broadcast media
enthusiastically promote new obstetrical technologies, medical interventions,
and now medically unnecessary cesareans. It would be
refreshing to see journalists question their questionable relationship with a faith-based reporting system
and instead ask real questions of the obstetrical profession.
Considering that:
-
maternity care is
20% of the national health care budget,
-
that 40% of all
births are paid for by the federal Medicaid program,
-
that many state governments are facing huge budget
deficients,
-
that bio-chemical
terrorism would overwhelm our current interventionist and drug intensive
obstetrical system --
maybe, just maybe,
normal or ‘physiological management’ by doctors and midwives as the
acknowledged standard for healthy women is an idea worth exploring.
The real
question for journalists is why
the majority of childbearing women do not receive the safer, cost-effective
and non-interventive type of care established as beneficial in the Guide to Effective Care in Pregnancy and Childbirth (synoptic
version of third edition) and recommended
by the highly respected Maternity Center Association of NYC.
The beneficial practices identified by the Guide
to Effective Care are protective and reduce medical and surgical
interventions and yet they are absent for the majority of women giving
birth in this country under obstetrical management.
The challenge for the 21st century is to bring
about a fundamental restructuring of maternity care in the
United States. This is an economic as well as a humanitarian
issue. Worldwide, the global economy depends on
the use of physiological principles and low-tech, inexpensive methods of midwifery care for normal birth
services to retain its competitive edge. The US must also utilize these safe
and cost-effective forms of care in order to compete in a global
economy. In the US the social model of childbirth, which depends
squarely on physiological
management for its success in providing care to healthy women with normal
pregnancies, must become the foremost standard of care. At least 70% of the childbearing population
is healthy and have normal pregnancies.
Under this system, management strategies would be
determined by the health status of the childbearing woman and her
unborn baby in conjunction with the mother’s stated preferences, rather than
by the occupational status of the care
provider (physician, obstetrician, midwife). At present, who the
woman seeks care from (doctor vs. midwife) determines how she is
cared for. Currently our tort laws force doctors to provide interventionist
care irrespective of the health status of the mother, or of her wishes. It
should be noted that this creates an asymmetrical burden of risk that falls
unfairly on the childbearing woman, in which the mother is exposed to the
actual pain and potential harm of medical and surgical interventions in order
to reduce the risk of lawsuits for the obstetrician. This is
unacceptable.
The unexamined theory of our tort laws induce physicians to
protect themselves by 'cost-shifting', 'risk-shifting' and 'blame
shifting'. This is particularly pernicious when surgical "solutions"
are implemented by obstetricians in order to reduce the legal culpability to
themselves, as physicians are not legally responsible for post operative
complications. For instance, physicians are expressly exonerated
liability for "downstream" sequelae or time-delayed complications such as
future incontinence (the sequelae of forceps delivery) or placenta percreta in a future
pregnancy (the sequelae of Cesarean section). Dr. Peter Bernstein made this observation earlier
when he note that the law (and at present the ethical designation by society) inappropriately
protects the physician who chooses to reduce the litigious risk to himself
by shifting it forward to the mother and/or baby in a future pregnancy.
According to Dr. Bernstein::
"There may be
no legal
liability to the physician who performed the patient's first cesarean section
when the patient winds up with a hysterectomy or worse, but that does not clear
that physician of responsibility for performing a surgical procedure of
unclear benefit...."
In the short term, the most direct remedy to this
problem is truly transparent informed consent for the use of interventive and
operative obstetrics. In the long term it requires the rehabilitation of two
important areas of modern life --our tort laws and of our maternity care
system.
In a rehabilitated maternity care system, physicians who
provide care to a healthy population would be required to either utilize the successful strategies
of physiological management themselves, cede the care of healthy women to
those who do, or obtain truly informed consent for substituting medicalized
obstetrical care with its well-documented dangers. Fully informed consent would require true informational transparency
relative to the documented consequences of medicalized labor and normal birth
conducted as a
surgical procedure.
Scientifically correct
information must be routinely provided on the limitations and problems
associated with the medicalization of
labor – i.e., drugs, anesthesia, and medical interventions and procedures that abnormally limit mobility or confine the laboring women to bed.
This severely limits or eliminates access to time-tested strategies of
physiological management and right use of gravity, thus increasing artificial
stimulation of labor and operative delivery and all their associated
complications.
Obstetricians must provide valid information during the last
trimester of pregnancy that includes the short and long
term complications
associated with major medical and surgical procedures performed
during the labor – continuous electronic fetal monitoring, restriction of oral nourishment,
IVs, labor stimulating/inducing drugs, off-label use of drugs (ex. Cytotec), narcotic
medication, epidural anesthesia, indwelling bladder catheters, episiotomy, vacuum extraction, forceps and a
26% cesarean section rate. The benchmark for this transparency should be the same
information about complications that is reported to physicians in the scientific
literature and obstetrical trade papers, such as Ob.Gyn.News. This
should be faithfully restated
for childbearing parents in
lay terms that are appropriate for their
concerns.
Electronic Fetal Monitoring ~
Institutionalized failure as an art form
In particular, obstetricians must identify the
lavishly-documented failure of continuous electronic fetal monitoring and liberal
use of cesarean section to reduce the rate of cerebral palsy and other
neurological disabilities. Most
people wrongly assume that EFM is the equivalent of an electrocardiogram
(EKG) for the unborn baby but this is a serious misunderstanding of the
technology. Electronic monitoring is simply an elaborate mechanism to count
the pulse of the unborn baby. The machine merely transposes the acoustic signal of
heart rate into a printed paper graph and video display, which makes the four
auditory markers of fetal well-being visible. The use of an acoustical fetascope or an
electronic doptone can provide the same on-going data (same four markers) on the well-being of the
unborn baby without the interpretive errors, physical
restrictions and unrealistic expectations associated with the use of continuous EFM.
In July of 2003, a report
by the ACOG Task Force on Neonatal Encephalopathy & Cerebral Palsy
stated that:
"Since the advent of fetal heart rate monitoring, there has
been no change in the incidence of cerebral palsy." "... The
majority of newborn brain injury does not occur during labor and delivery.
Instead, most instances of neonatal encephalopathy and cerebral palsy are
attributed to events that occur prior to the onset of labor."
This
report had the endorsement and support of six major federal agencies and
professional organizations, including the Center for Disease Control &
Prevention (CDC), the March of Dimes and the obstetrical professions in
Australia, New Zealand and Canada. It is described as the "most
extensive peer-reviewed document on the subject published to date."
An August 15, 2002 report on this topic in Ob.Gyn.News stated that
"performing cesarean section for abnormal fetal heart rate pattern in an
effort to prevent cerebral palsy is likely to cause as least as many bad
outcomes as it prevents." "... A physician would have to
perform 500
C-sections for multiple late decelerations or reduced beat-to-beat
variability to prevent a single case of cerebral palsy."
The
September 15, 2003 edition of Ob.Gyn.News stated
that:
"The
increasing cesarean delivery rate that occurred in conjunction with fetal
monitoring has not been shown to be associated with any reduction
in the CP rate..." " ... Only 0.19% of all those in the study
had a non-reassuring fetal heart rate pattern.... If used for identifying
CP risk, a non-reassuring heart rate pattern would have had a 99.8% false
positive rate...."
Despite
a success rate of only 00.2%, most hospitals bill around $400 an hour
for continuous EFM. Regularly listening to fetal heart tones with an electronic Doppler
for one
full minute immediately after a contraction, (called Intermittent auscultation
or ‘IA’) permits the same data on the four
auditory markers of fetal well-being (baseline heart rate, variability,
accelerations and absence of pathological decelerations) to be obtained. While intermittent
auscultation is more time-intensive, IA for low and
moderate-risk labors is equally as effective as continuous EFM, with the added benefit of a greatly reduced cesarean rate (4% vs. 26%). This
is, in part, because it unhooks healthy mothers from machines and
permits laboring women to move around freely. No longer tethered to the bed by
electronic wires, the mother is able to change positions frequently,
walk, use hot showers or deep water for pain relief and make “right use of
gravity” These practices reduce fetal distress and the need for Pitocin-augmentation of
labor, pain medication, anesthesia and instrumental and operative delivery.
Obstetricians need to acknowledge this domino effect, also called the cascade of
interventions, associated with highly medicalized childbirth. This cascade
occurs when procedures, such as induction of labor, trigger the need for other
interventions, such as continuous EFM and epidural anesthesia. The cascade of
interventions can
so disturb the biological process that it can in turn lead to
fetal distress or operative
interventions. Cesarean section is the ultimate operative intervention and is
associated with a peripartal emergency hysterectomy rate 13 times greater than
vaginal birth. Other
common surgical interventions such as episiotomy, forceps and vacuum extraction are strongly associated with pelvic organ dysfunction and maternal
incontinence after the birth. These pelvic floor problems are not, as some
obstetricians claim, merely collateral damage of normal birth but are the
predictable consequence of a failure to make
right use of physiological principles, especially spontaneous labor and the right use of
gravity.
Medical journals make it clear to all that routine obstetrical
interventions and birth as a surgical procedure for healthy
women are always more dangerous than the use of
physiological principles in conjunction with appropriate social and psychological
support. Scientifically-speaking, this is not a controversial finding.
Reliable scientific evidence is neither lacking nor incomplete, nor is this
data the subject
of methodological disputes.
Consider this: If planes landing at US airports crashed
five times more often than when they landed at airports in England or Japan,
we would demand an inquiry of our air traffic control system, since the laws
of aerodynamics are the same worldwide. Each year in the US about 8 million mothers and
babies 'fly' ACOG's united service of interventionist obstetrics.
Only a fraction -- under 30% -- need and benefit from this type of
medicalized treatment. Isn't it time to inquire why the universal 'laws
of normal childbirth,' which are the same worldwide, are being routinely
suspended by American obstetricians and, as a result, American mothers
and babies are crash landing at an alarming rate.
|
Chapter Six |
 |
| ~
How to Make the System work for everyone |
The main and the plain reading of the scientific
literature brings one to the logical conclusion that physiological
management is the safer and most cost-effective form of care for a healthy
population. This leads us to the natural and compelling conclusion that our current hospital-based maternity care system
must be rehabilitated.
A newly formulated national health care policy would integrate physiological principles with the best advances in obstetrical
medicine to create a single, evidence-based standard for all
healthy women. That standard must be based on
criteria arrived at through an interdisciplinary process that INCLUDES
the traditional discipline of midwifery as an independent
profession and
integrates the input of childbearing women and their families into the
process. It is especially important to include testimony from those
families who had complications following cesarean surgery or who found it virtually impossible to
arrange for a subsequent normal labor and birth after a cesarean (VBAC). Such a transformation in our national maternity care
policy would require that:
-
Medical educators learn and teach the principles of
physiological management to medical students, interns and residents
-
Practicing physicians learn and utilize these same skills
-
Fully informed consent for obstetrical
management of healthy women be provided that includes true informational
transparency
relative to the documented consequences of medicalized labor and normal birth
conducted as a
surgical procedure.
-
Hospital labor & delivery units be primarily
staffed by professional midwives,
with incentives for current L&D nurses who wish to retrain for
hospital-based midwifery practice to do so at minimal expense to
themselves
-
Third party payers fairly reimburse all practitioners for the
professional's time spent facilitating normal childbirth, which helps
avoid the need for medical
and surgical intervention, as well as reimbursing for medical and surgical
procedures
-
Tort law (medical malpractice)
reform be enacted so that doctors are not inappropriately judged by outdated
medical
criteria that are not evidence-based
In a
rehabilitated maternity care system, professional midwives, family practice
physicians and obstetricians would all enjoy a mutually respectful,
non-controversial relationship. Appropriate maternity care would be provided by all three
categories of professionals
in all three birth settings as appropriate – hospital, home and birth center – without
prejudice, controversy or retaliation against the childbearing family or
against other care providers. By making maternity care in all settings equally safe and equally satisfactory, families
would not be forced to submit to forms of care that are not appropriate for their
needs or that waste our economic resources.
This rehabilitative process could be launched by the California state legislature or a public policy organization such as the Pew
Charitable Trust which could convene a blue-ribbon panel consisting of scientists from all the pertinent disciplines – public health,
epidemiology, sociology, anthropology, psychology, biology, child development, law, economics, midwifery, perinatalogy and
obstetrics. Such a highly respected forum would study these
problems and provide unbiased, fact-based news for the press and
broadcast media to report. This public exploration must include listening to childbearing women and their families as
a class of experts in the maternity experience.
Such a panel would produce
interdisciplinary recommendations for a reformed national maternity care
policy. This would include methods to reintegrate midwifery
principles and practice into this expanded system of maternity care.
Ultimately such exploration and recommendations would result in legal and legislative changes affecting doctors,
hospitals, midwives and the health insurance industry.
Such a system would then be respected and used equally
by all maternity care providers with the backing of hospitals,
health insurance and medical malpractice carriers, and state and federal
reimbursement systems (Medicaid / MediCal) etc.
|
 |
Only by returning the philosophy and physiological
principles of normal childbearing to their rightful and central place in our
national maternity care policy can our healthcare system economically meet the
needs of our own childbearing population while remaining competitive in the
global economy of a 21st century world. |
Link to: Lancet 2000; 356: 1677-80
Choosing
Caesarean Section
by Dr. Marsden Wagner, MD, MSPH
(formerly World Health Organization's director of maternal-infant health for
32 European countries
=============================================================================================
Editorial
~ Home Delivery -- Why? Michael Fleming, MD, Assistant
Professor,
Department of Family Medicine, School Medicine, University of North Carolina,
Chapel Hill
This editorial gives an excellent
perspective by a family practice physician on why and how to employ
physiological principles in hospital-based obstetrical practice, including the
full-time presence of the
primary caregiver during active labor (also
see "Physiologically-sound practices" immediately below)
=============================================================================================
Index
Page for Citations,
Abstracts, Excerpts and Quotes
from eObGynNews.com
and other respected sources of professional information
on safety, complications & practice trends for obstetricians
Stedman’s
Medical Dictionary definition of “physiological” – “…in accord with,
or characteristic of, the normal functioning of a living organism”
(1995)
Physiologically-sound
practices (midwifery principles of care) include:
Continuity of
care
Patience with nature
Social and emotional support
Mother-controlled environment
Provision for appropriate psychological privacy
Mother-directed activities, positions & postures for labor &
birth
Full-time presence of the primary
caregiver during active labor
Recognition of the
sexual nature of spontaneous labor
Upright and mobile mother during active labor
Non-pharmaceutical pain management such as showers & deep water tubs
Judicious use of drugs and anesthesia when needed
Absence of arbitrary time limits as long reasonable progress, mom & babe
OK
Vertical postures, pelvic mobility and the right use of
gravity for pushing
Birth position by maternal choice unless other factors require
otherwise
Mother-Directed
Pushing / NO Valsalva Maneuver
(prolonged
breath-holding)
Physiological clamping/cutting of
umbilical cord-- after circulation has stopped (+/-3 minutes)
Immediate possession and control of newborn by mother and father
On-going & unified care and support of the mother-baby for postpartum
Access to appropriate care for the 'Second Nine Months' -- breastfeeding advise,
infant development, parenting and
psychological adjustments to postpartum stresses
relative to other children,
spouse and employment outside the home, etc
One does not have to be a midwife to appropriately
use physiological (i.e. "midwifery") management.
Return
to College of Midwives' homepage
Most readers will remember the amazing picture of African
woman and her newborn baby being rescued by helicopter from in a tree. Nine
months pregnant and trapped by rising flood waters for 3 days, she gave birth
without human assistance in the upper branches of tree. Mother and baby were
both healthy. This reflects the genetic success of our reproductive biology.
link to single page